*This post may contain affiliate links for which I earn commissions.*
Diabetes, at its core, is a condition that affects how the body processes blood sugar (glucose). Glucose is crucial because it’s a significant energy source for cells that make up muscles and tissues and the primary fuel for the brain. Worldwide, diabetes is on the rise. According to the International Diabetes Federation, 537 million adults globally have diabetes. Based on an estimated population figure of 8 billion, 11.2% of the global population has diabetes. While the condition itself does not directly “kill,” its long-term effects can severely damage vital organs, including the heart, kidneys, eyes, and nervous system. Chronic high blood sugar levels increase the risk of heart disease, stroke, kidney failure, and infections that are harder to fight off, especially in cases of Type 2 diabetes. In addition, diabetic ketoacidosis—a life-threatening condition in Type 1 diabetes—can result from insufficient insulin, leading to a rapid and dangerous spike in blood sugar. However, with proper medical care, a healthy lifestyle, and regular monitoring, diabetes can be managed, greatly reducing the risk of fatal outcomes.
Diabetes My full disclosure.
I have never been a diabetic and I have never had raised sugar levels, partly down to genetics and partly down to the fact that I eat a very nutrient dense diet. Having said that, my husband was diagnosed with type 2 diabetes when he was about 58. All went well. He took to heart that it was a lifelong disease, and he had to take the medicine. (Despite me telling him there was a growing number of research cases coming out of Northumberland University in the UK that that view was nonsense.)
Anyway, after two years, he was told he would have to start giving himself insulin injections daily. He was on four metformin a day, and that was the maximum dose, but his sugar levels were dangerously high. I said that, together, we could work on him weaning himself off all medication. I think the poor lad was terrified of injecting himself. As is often the case, he was catapulted into a lifestyle change. It took just days to see a dramatic drop in his sugar levels. Within four days, they had dropped by a third, and within 6 weeks, he was medication free. He remained free of medication until his death ten years later.
So, I came to know a great deal about what life was like for a diabetic. I know it changes how you look at the world. I understand his terror at getting nerve damage. I had to live with the fact he was obsessed with his feet and examined them daily.
Diabetes
There are three main types of diabetes: Type 1, Type 2, and gestational. Type 1 is usually diagnosed in children and young adults. In this type, the body doesn’t produce insulin, a hormone needed to get glucose from the bloodstream into the cells. Type 2, the most common type, generally develops in adults and is often linked to lifestyle choices. It occurs when the body can’t use insulin properly. Gestational diabetes happens during pregnancy and typically resolves after giving birth, but it needs close monitoring as it might affect both mother and baby.
The Pathophysiology of Diabetes
Diabetes impacts several aspects of the body’s functioning, starting with how it deals with insulin and glucose. Insulin, a hormone produced by the pancreas, helps cells take in glucose, which provides energy. When someone has diabetes, this process doesn’t work as it should.
In Type 1 diabetes, an autoimmune reaction occurs, where the body attacks and destroys insulin-producing cells in the pancreas. This means little to no insulin is produced, leading to high blood sugar levels. Since the body can’t create insulin, people with Type 1 diabetes need daily insulin injections or an insulin pump to manage their blood sugar.
Type 2 diabetes is a bit different. The body becomes resistant to insulin over time, meaning it doesn’t use the hormone efficiently. The pancreas tries to compensate by producing more insulin, but eventually, it can’t keep up, resulting in elevated glucose levels. This can go unnoticed for years, so regular check-ups are crucial. Back in the day, in the sixties, it was known as the silent killer. There were fewer cases then, and they often went undiagnosed for many years.
When blood sugar levels are too high over prolonged periods, it can cause significant damage. This damage affects the heart, blood vessels, nerves, eyes, and kidneys. However, the symptoms might not be obvious at first. Some early signs include increased thirst, frequent urination, fatigue, and blurred vision. Recognizing these symptoms early can lead to timely intervention and better management.
Managing blood sugar levels helps prevent these complications. This involves regular monitoring through blood tests, adopting a healthy diet, and, if needed, taking medication as prescribed by a doctor. If you have any concerns or symptoms related to diabetes, talking to a healthcare professional is a wise step.
Short-Term Health Risks of Diabetes
When managing diabetes, it’s important to be aware of the short-term health risks that can arise. Two common issues are hypoglycemia and hyperglycemia. Hypoglycemia, or low blood sugar, happens when blood sugar levels drop too low. It can cause symptoms like shakiness, sweating, confusion, and even loss of consciousness if not addressed promptly. To prevent hypoglycemia, people with diabetes should regularly monitor their blood sugar, eat meals consistently, and carry glucose tablets or snacks as a quick fix.
On the flip side, hyperglycemia, or high blood sugar, occurs when blood sugar levels are too high. This condition can make you feel extremely thirsty, cause frequent urination, and lead to problems like nausea and dizziness. If not managed, hyperglycemia can escalate to diabetic ketoacidosis (DKA), especially in those with Type 1 diabetes. DKA is a severe condition where the blood becomes acidic due to high levels of ketones. Symptoms include rapid breathing, fruity-smelling breath, and severe dehydration. Immediate medical attention is necessary to treat DKA.
Infections are another concern for diabetics. High blood sugar can weaken the immune system, making it easier for infections to take hold. Common infections among people with diabetes include skin infections, urinary tract infections, and gum disease. Moreover, wounds and cuts can take longer to heal, increasing the risk of complications. Practicing good hygiene, keeping blood sugar levels in check, and seeking medical advice at the first sign of infection are crucial steps to mitigate these risks.
Keeping track of these potential short-term health issues and managing them effectively is a big part of living well with diabetes. Consistent blood sugar monitoring, and a proactive approach to health can make a real difference. If symptoms of hypoglycemia or hyperglycemia arise, addressing them promptly is key to preventing more serious complications.
Long-Term Health Complications
Living with diabetes means being mindful of long-term health complications that can arise. One significant risk is cardiovascular disease. High blood sugar levels over time can lead to the buildup of fatty deposits in blood vessel walls, causing narrowing and hardening of the arteries. This increases the risk of heart attacks and strokes. Regular check-ups with a healthcare provider, along with a heart-healthy diet and exercise routine, can help mitigate these risks.
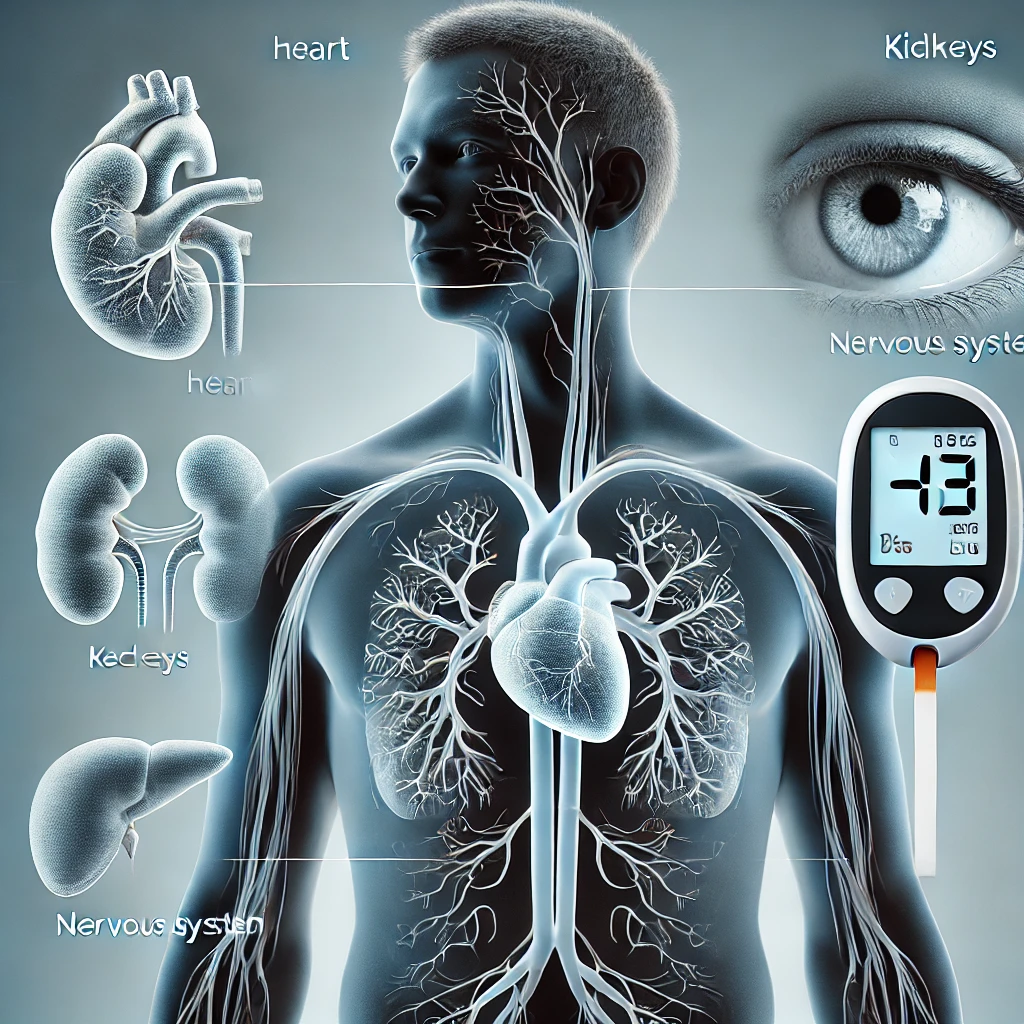
Nerve damage, or neuropathy, is another common complication. High glucose levels can damage nerves, especially in the legs and feet. Symptoms include pain, tingling, or loss of sensation. This can make it easier to get infections or wounds unnoticed. Proper foot care, including regular checks and wearing comfortable shoes, is essential to prevent issues from escalating.
Kidney damage, known as nephropathy, can also occur. The kidneys filter waste from the blood, but high sugar levels can damage this filtering system. Over time, this may lead to kidney failure. Regular urine tests to check for albumin, a type of protein, can help in the early detection of nephropathy. Maintaining blood pressure and sugar levels within target ranges is crucial for kidney health.
Vision problems, particularly diabetic retinopathy, are another concern. This condition affects the blood vessels in the retina and can lead to vision loss if not treated. Regular eye exams are essential to catch any changes early. Controlling blood sugar and blood pressure can greatly reduce the risk of retinopathy.
Foot problems are also common among diabetics and can sometimes lead to amputations if infections or ulcers go untreated. Keeping feet clean and moisturized, avoiding tight-fitting shoes, and inspecting feet daily can help catch problems early. Prompt treatment of any foot infections or sores is critical.
Being proactive in managing these long-term complications makes a big difference. Regular health check-ups, monitoring blood sugar levels, and following medical advice can help prevent or delay these issues. If you notice any new symptoms or changes in your health, reaching out to your healthcare provider is a wise move.
Does Diabetes Increase Mortality Risk?
When discussing diabetes, it’s vital to consider whether it increases the risk of mortality. Statistics show a clear connection between diabetes and a higher risk of death. According to the World Health Organization, diabetes was directly responsible for 1.5 million deaths in 2019. Many more deaths were indirectly linked to high blood glucose levels, which contributed to the development of cardiovascular disease and other conditions.
Several factors influence this increased mortality risk. Poorly managed blood sugar levels can lead to both acute complications like diabetic ketoacidosis and chronic conditions such as heart disease and kidney disease. Additionally, the longer someone lives with diabetes, the higher the likelihood of developing serious complications.
Comparing diabetes with other chronic diseases gives further insight. While conditions like hypertension and high cholesterol also pose significant health risks, the unique aspect of diabetes is its direct impact on multiple organs and systems in the body. This makes it a multifaceted threat requiring comprehensive management strategies.
However, it’s worth noting that well-managed diabetes significantly reduces the risk of mortality. Advances in medical treatments, technologies like continuous glucose monitors, and better education on managing the condition all contribute to healthier and longer lives for those with diabetes. Regular monitoring, medication adherence, a balanced diet, and regular physical activity play crucial roles in mitigating risks.
In summary, while diabetes does increase the risk of mortality, the emphasis should be on prevention and effective management. Early diagnosis, vigilant management, and support from healthcare providers are key to reducing the risks associated with this condition.
Preventative Measures and Management
The Role of Diet in Managing Diabetes.
Managing diabetes effectively involves a combination of lifestyle changes, medication, and regular monitoring. It all starts with adopting healthier habits. Diet plays a huge role in controlling blood sugar levels. Focusing on a balanced diet rich in vegetables, lean proteins, whole grains, and healthy fats can make a big difference. Avoiding sugary beverages and processed foods is also crucial.
I have to state that there is no one-size-fits-all diabetic diet. My husband was told that brown rice was good for diabetes. Because he was obsessive about checking his sugar levels after eating in the first year. We found out that nothing, absolutely nothing, drove his sugar levels up like brown rice.
The Role of Exercise in Managing Diabetes.
Exercise is another cornerstone of diabetes management. Engaging in regular physical activity helps the body use insulin more efficiently, lowers blood sugar levels, and boosts overall health. Aim for at least 150 minutes of moderate-intensity aerobic activity each week, like brisk walking or cycling. Strength training exercises a couple of times a week are also beneficial.
Is Medication Mandatory for diabetics
In addition to lifestyle changes, medication often plays a role in diabetes management. People with Type 1 diabetes will need insulin therapy, while those with Type 2 diabetes might be prescribed oral medications or insulin, depending on their condition. It’s important to follow the treatment plan provided by your healthcare provider and discuss any concerns or side effects you experience.
Regular monitoring and check-ups are essential. Keeping track of blood sugar levels helps you and your healthcare team make informed decisions about your treatment plan. Investing in a good quality blood glucose monitor and using it as directed can provide valuable insights into how different foods and activities affect your blood sugar.
“Diabetes is a disease of complications, and those complications are what we’re trying to prevent.”
Dr. Griffin P. Rodgers
Managing Stress
Managing stress is equally important. Stress can impact blood sugar levels, so incorporating stress-reducing activities like yoga, meditation, or even simple breathing exercises can be beneficial. Additionally, adequate sleep supports overall health and well-being.
Preventing complications means staying proactive. Regular check-ups, eye exams, and screenings for kidney function and heart health can catch issues early before they become serious. If you smoke, quitting is one of the best steps you can take to improve your health and manage diabetes effectively.
Innovations and Research in Diabetes Treatment
Recent advancements in diabetes treatment show promising results. New medications are continually being developed. These aim to control blood sugar more effectively with fewer side effects. Some of the latest medications work by targeting different pathways in the body, offering additional options for people who may not have responded well to traditional therapies.
Advances in technology have revolutionized diabetes management. Continuous glucose monitors (CGMs) now provide real-time blood sugar readings, reducing the need for frequent finger pricks. These devices can alert users to dangerous highs and lows, making it easier to maintain stable blood sugar levels. In addition to CGMs, insulin pumps have become more sophisticated. Closed-loop systems, also known as artificial pancreases, can automatically adjust insulin delivery based on glucose readings, significantly reducing the burden of constant monitoring and manual insulin administration. Blood sugar support is now available
Glucocil – Premium Blood Sugar Support – Over 2 Million Bottles Sold – Supports The 3 Essentials for Healthy Blood Sugar – Since 2008, with Berberine, Proprietary Mulberry Leaf, and More
FULL SPECTRUM OF BENEFITS TO SUPPORT BLOOD SUGAR HEALTH: (1) Supports healthy blood sugar levels, (2) Supports healthy weight management, (3) Supports healthy sugar & carb absorption, (4) Supports heart health, and (5) Supports healthy energy.
Research into potential cures for diabetes is also progressing. Scientists are exploring various approaches, such as beta cell replacement and immune system modulation. Beta cell replacement involves transplanting insulin-producing cells into the body to restore natural insulin production. Immune system modulation aims to prevent the immune system from attacking insulin-producing cells, particularly relevant for Type 1 diabetes. While these treatments are still in experimental stages, they offer hope for a future where diabetes can be cured or significantly better managed.
Getting involved in clinical trials is another way to contribute to this progress. Many hospitals and research institutions offer opportunities to participate in studies that test new treatments. Not only does this contribute to the broader scientific understanding of diabetes, but it also provides access to cutting-edge therapies before they are widely available.
Staying informed about the latest research and advancements in diabetes treatment can empower you to make better decisions about your health. Discussing these options with your healthcare provider ensures that you receive the most current and effective treatments available.
Living with Diabetes: Personal Stories and Support
Personal stories offer a unique perspective on managing diabetes. Hearing from others who live with the condition can provide comfort, inspiration, and practical advice. Every person’s journey with diabetes is different, and sharing these experiences sheds light on various ways to cope and thrive.
Support groups and communities play a crucial role. Connecting with others who understand the challenges of diabetes can be incredibly beneficial. Whether online or in-person, these groups offer a space to share experiences, ask questions, and receive emotional support. It can be reassuring to know that you’re not alone in your journey.
Managing diabetes often extends beyond just physical health—it can take a toll on mental well-being too. Coping with chronic illness can lead to stress, anxiety, and even depression. It’s important to address these mental health concerns with the same seriousness as physical symptoms. Speaking with a therapist or counselor can offer valuable tools and strategies for handling the emotional aspects of diabetes.
Family and friends also play a vital role in supporting those with diabetes. Educating them about the condition helps build a stronger support network. Simple actions, like preparing healthy meals together or joining in exercise routines, can make a significant impact. Encouraging loved ones to understand the daily challenges of diabetes fosters empathy and provides much-needed encouragement.
Educational resources are abundant and can help you stay informed. Books, reputable websites, and diabetes education programs offer a wealth of information on managing the condition. Staying informed helps you make empowered decisions about your health care and keeps you up-to-date with new treatments and research.
Everybody’s path with diabetes is unique, but you don’t have to navigate it alone. Utilize the power of community, seek help when needed, and arm yourself with knowledge. Sharing your journey with others and learning from their experiences can pave the way to better management and a fuller life.
Managing Diabetes for a Healthier Life
Living a healthy life with diabetes is entirely achievable. Effective management involves a combination of smart choices, regular monitoring, and emotional support. It means taking charge of your health with a proactive mindset.
Regular health check-ups can play a vital role. These visits allow for early detection of potential complications and enable adjustments to your treatment plan. Consistent monitoring of blood sugar levels offers insights into hobut you do not have to live in the w your daily habits impact your condition, empowering you to make informed decisions. While I am not saying do not have these check-ups, remember that healthcare professionals around the world get paid every time you visit them. Drug companies often pay them. My advice would be to take a proactive approach and decide for yourself how often you need a visit. Managing diabetes is crucial, but nothing is stopping you from doing that yourself. A certain amount of health checks are mandatory but you don’t have to live in a doctor’s surgery
Diet and exercise cannot be overstated. Prioritizing a balanced diet and consistent physical activity significantly affects your blood sugar management and overall well-being. Whether it’s experimenting with new nutritious recipes or finding physical activities you enjoy, these lifestyle habits are cornerstone practices in diabetes care.
Mental well-being is equally important. Stress management techniques such as mindfulness, meditation, or even hobbies that bring joy can make a world of difference. Emotional support from family, friends, and support groups adds another layer of strength, making challenges easier to navigate.
Staying informed about medical advancements and treatment options is crucial. Engaging in continuous education about diabetes can help you take advantage of the latest research and innovations, enhancing your management strategies.
Remember, each step towards better management counts. Small, consistent changes in your daily routine can lead to significant improvements over time. Arm yourself with knowledge, seek support when needed, and remain hopeful. Living well with diabetes is not just a possibility; it’s within your reach.
In Conclusion, Does Diabetes Kill?
While diabetes itself rarely leads directly to death, the complications it can cause are both life-threatening and challenging. Uncontrolled blood sugar levels can result in serious health issues such as heart disease, kidney failure, nerve damage, and infections that can escalate quickly without proper management. The key to minimizing these risks lies in consistent monitoring, a healthy lifestyle, and appropriate medical care. By taking proactive steps to manage diabetes, many people can lead long and healthy lives, significantly reducing the chance of facing these dangerous complications. Diabetes is a leading cause of non-traumatic limb amputations, primarily due to complications such as peripheral artery disease (PAD) and diabetic neuropathy, which can lead to severe foot ulcers and infections. Individuals with diabetes are 10 to 20 times more likely to undergo amputation compared to those without the condition. About 1 in 6 people with diabetes will experience a foot ulcer at some point in their life, and of those, 1 in 5 will require an amputation. Put simply, one in 6 diabetics will have a foot amputated.
Frequently Asked Questions About Does Diabetes Kill?