*This post may contain affiliate links for which I earn commissions.*
Insulin resistance occurs when cells in the body don’t respond well to insulin, a hormone that helps glucose from the blood enter cells to be used for energy. This means the pancreas needs to produce more insulin to help keep blood sugar levels in check. Over time, this increased demand on the pancreas can lead to the development of type 2 diabetes.Several factors contribute to insulin resistance. Genetics plays a significant role. If your family has a history of diabetes or related conditions, you might be at higher risk. Lifestyle choices like a high-sugar diet, lack of physical activity, and obesity also heavily impact insulin sensitivity. Hormonal imbalances and certain medical conditions can also be contributing factors.
Insulin Resistance And Diabetes are Two Different things
It’s crucial to understand that insulin resistance and diabetes aren’t the same thing. Insulin resistance means your body isn’t using insulin effectively, but your blood sugar levels might still be within a normal range because your pancreas is compensating by making more insulin. Diabetes occurs when this compensation can no longer keep up, leading to consistently high blood sugar levels. Insulin resistance does not always lead to diabetes. While insulin resistance is a significant risk factor for developing type 2 diabetes, it doesn’t guarantee that diabetes will occur.
The Early Signs of Insulin Resistance
Recognizing the early signs of insulin resistance can be tricky since symptoms often go unnoticed. A common sign is increased hunger, especially after eating. This happens because your body struggles to move glucose into your cells, and insulin facilitates that exchange. This leaves you feeling hungry even though you’ve just eaten.
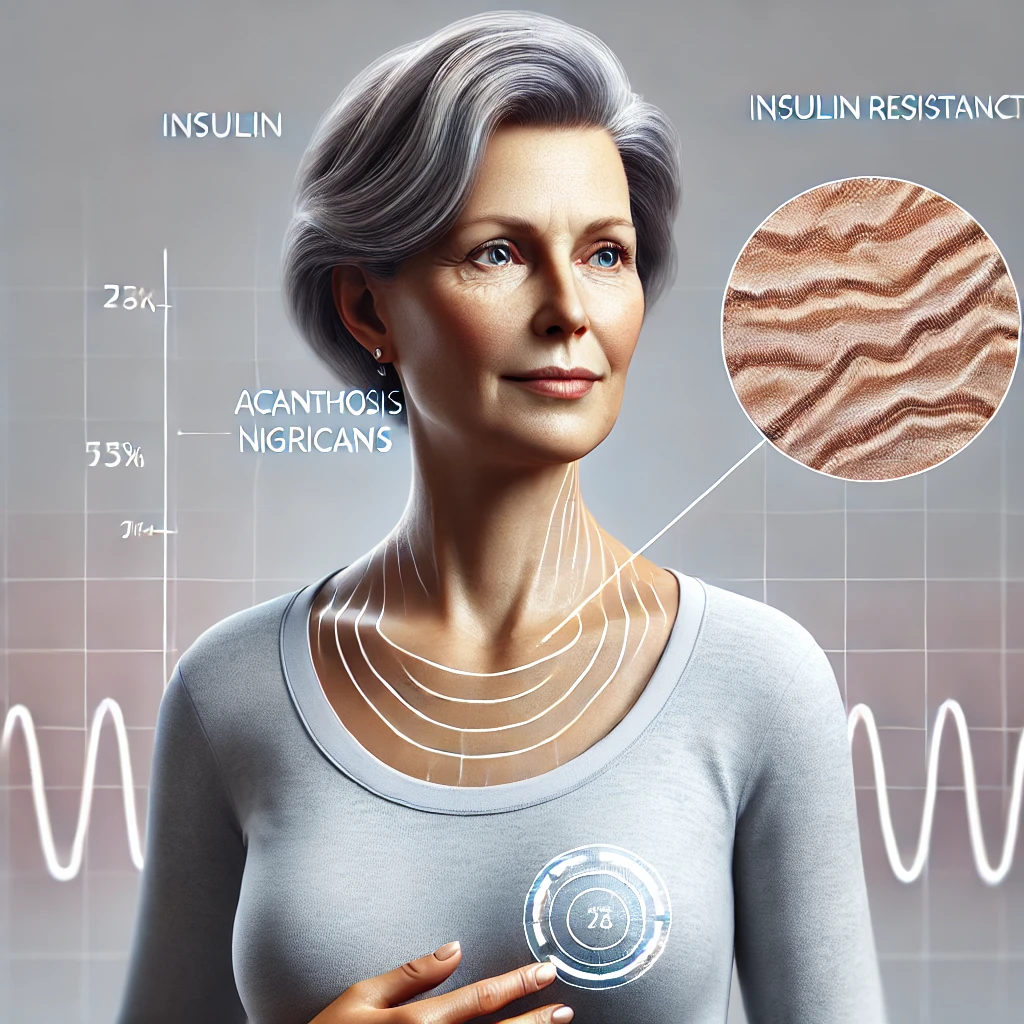
Another red flag is unexplained weight gain, particularly around the abdomen. High insulin levels can prompt the body to store more fat, especially in the midsection. Skin changes, like dark patches on the neck or underarms (a condition called acanthosis nigricans), can also indicate insulin resistance.
Fatigue is common, too. Because your cells aren’t getting the energy they need from glucose, you might feel constantly tired even with adequate sleep. This fatigue can be accompanied by brain fog or difficulty concentrating.
Regular medical tests, such as fasting glucose, HbA1c, and insulin levels, can help diagnose insulin resistance. Knowing your numbers enables you to take proactive steps to manage your health, even if you don’t feel any symptoms yet. Always consult with a healthcare provider for accurate diagnosis and tailored advice.
Who is at Risk?
Genetics plays a significant role in developing insulin resistance. If you have a family history of type 2 diabetes, you might be more prone to this condition. However, lifestyle choices and environmental factors are just as crucial.
Lifestyle factors such as a diet high in processed sugars and unhealthy fats significantly increase your risk. Lack of physical activity is another big contributor. Regular exercise helps your cells respond better to insulin, so a sedentary lifestyle can make insulin resistance more likely.
Age is another factor to consider. Insulin resistance tends to increase as you get older. Hormonal changes, particularly during menopause, can also make women more susceptible.
Certain medical conditions and medications can elevate your risk too. Conditions like polycystic ovary syndrome (PCOS) and sleep apnea are linked to higher rates of insulin resistance. Some prescription drugs, such as steroids, can also interfere with how your body processes insulin.
Being overweight or obese, especially having excess fat around the abdomen, raises your risk significantly. This abdominal fat is particularly harmful because it produces hormones and other substances that can lead to inflammation and insulin resistance.
Gender also plays a role. Men are generally more likely to develop insulin resistance than women, up until women reach menopause. After menopause, women’s risk can equal or surpass that of men.
Insulin Resistance: A Pathway to Diabetes?
Insulin resistance and diabetes are closely linked, but having insulin resistance doesn’t mean you’ll definitely develop diabetes. Many people live with insulin resistance for years without ever developing type 2 diabetes. The key lies in understanding how and why the transition can happen.
When your body becomes resistant to insulin, the pancreas compensates by producing more of it. Over time, this overproduction can exhaust the beta cells in your pancreas. Beta cells are responsible for insulin production, and their failure is a significant factor in the onset of type 2 diabetes.
Studies show that not everyone with insulin resistance will develop diabetes. Lifestyle plays a massive role in this transition. Factors like a healthy diet rich in fiber, regular exercise, and maintaining a healthy weight can help prevent the progression to diabetes.
The role of beta cells in diabetes development can’t be overstated. Once these cells start to fail, your blood sugar levels begin to rise, leading to prediabetes and, eventually, type 2 diabetes if not managed effectively. Early intervention can save your beta cells from burning out, making early detection and management crucial.
Researchers are diving into the genetic and molecular aspects of this transition, aiming to identify markers that could predict who is more likely to progress from insulin resistance to diabetes. Ongoing research continues to improve our understanding of this complex relationship, offering hope for new interventions and preventative strategies.
Complications Beyond Diabetes
Insulin resistance doesn’t only increase the risk of diabetes; it also brings a host of other complications that can seriously impact quality of life. Cardiovascular issues are a significant concern. High levels of insulin can cause the walls of your arteries to thicken, leading to high blood pressure. This increases the risk of heart disease and stroke.
Fatty liver disease is another condition often linked with insulin resistance. It occurs when fat builds up in the liver, leading to inflammation and potentially severe liver damage over time. If left untreated, it can progress to cirrhosis or liver failure.
Chronic inflammation is frequently associated with insulin resistance. It contributes to many health issues, including atherosclerosis (hardening of the arteries), and plays a role in the development of certain cancers.
Renal complications are also common. The kidneys bear the brunt of high blood sugar levels and elevated insulin, which can lead to chronic kidney disease over time. Keeping an eye on kidney function is essential for those with insulin resistance.
Hormonal imbalances, especially in women, can be an additional complication. Conditions like polycystic ovary syndrome (PCOS) are frequently linked to insulin resistance and can cause issues like irregular menstrual cycles, infertility, and other metabolic problems.
Long-term, poorly managed insulin resistance can significantly affect mental health. High insulin levels and blood sugar fluctuations can contribute to anxiety and depression, highlighting the importance of a holistic approach to managing this condition.
Prevention Strategies
Changing your diet can make a significant difference in preventing insulin resistance. Focus on whole foods like vegetables, fruits, lean proteins, and whole grains. Avoid processed sugars and refined carbs that can spike your blood sugar levels.
Physical activity is essential. Regular exercise helps your muscles use glucose more efficiently, improving insulin sensitivity. Aim for at least 30 minutes of moderate exercise most days of the week. This can be anything from brisk walking to swimming or cycling.
Weight management is crucial. Carrying excess weight, especially around your midsection, increases your risk of insulin resistance. A combination of a balanced diet and regular exercise can help you maintain a healthy weight.
Adequate sleep and stress management are often overlooked but vital. Poor sleep and chronic stress can lead to hormonal imbalances that exacerbate insulin resistance. Aim for 7-8 hours of quality sleep per night and find healthy ways to cope with stress, such as meditation or yoga.
Regular monitoring of blood sugar levels and routine check-ups with your healthcare provider can help catch insulin resistance early. Early detection means you can implement lifestyle changes promptly, reducing the risk of complications.
Managing Insulin Resistance
Medications can be an effective way to manage insulin resistance, particularly when lifestyle changes alone aren’t enough. Metformin is commonly prescribed to improve insulin sensitivity. Your healthcare provider may also recommend medications that help control blood sugar levels or address related conditions such as high blood pressure or cholesterol.
Regular medical monitoring is vital. Frequent check-ups allow your healthcare provider to track your progress and make adjustments to your treatment plan as needed. This usually includes regular blood tests to monitor glucose levels, HbA1c, and other markers of metabolic health.
Personal stories of managing insulin resistance can be inspiring. Hearing how others have successfully managed their condition through lifestyle changes, medication, or a combination of both can provide motivation and practical tips. Many find success by creating a balanced approach that works for their unique situation.
Incorporating a supportive network can also make managing insulin resistance easier. Whether it’s through support groups, friends, or family, having a team behind you can help you stay on track and navigate the emotional challenges that often come with managing a chronic condition.
Emerging Treatments and Research
Innovative treatments are on the horizon for managing insulin resistance. Researchers are exploring medications that target the root causes, not just the symptoms. These therapies aim to improve how cells respond to insulin without overworking the pancreas.
One of the most promising areas of research is in gene therapy. Scientists are studying how to modify genes that affect insulin sensitivity, which could revolutionize how we treat insulin resistance in the future.
Hormone-based treatments are another exciting development. These therapies investigate how to balance other hormones in the body to improve insulin function, potentially offering new avenues for management.
Gut health has also become a focal point in recent research. The gut microbiome plays a significant role in metabolic health, and researchers are exploring probiotics and other treatments that could positively influence insulin sensitivity.
Clinical trials are essential in bringing these innovative therapies to the public. Participating in a trial could give you access to emerging treatments while contributing to scientific knowledge.
Staying informed about ongoing research is crucial. New findings can offer hope and provide new ways to manage insulin resistance more effectively in the long term. Keeping an eye on how scientific advancements evolve can give you more options and better management strategies.
Living Well with Insulin Resistance
Building a strong support system is key to managing insulin resistance effectively. Friends, family, or support groups can offer emotional and practical help, making it easier to stick to your treatment plan. They provide encouragement, share in your challenges, and celebrate your successes, helping to keep you motivated.
Mental and emotional well-being is just as important as physical health when dealing with insulin resistance. Techniques like mindfulness, meditation, or even talking to a therapist can help manage stress and reduce anxiety, leading to better overall health. Staying positive and proactive in your approach makes a significant difference.
Inspiring stories from individuals who live well with insulin resistance can provide practical tips and much-needed motivation. These stories can show you that it’s possible to thrive despite the condition, offering examples of successful management through lifestyle changes, medication, and support networks.
Remember, living with insulin resistance is a journey, and it’s okay to seek help along the way. Your healthcare provider, dietitian, or personal trainer can offer professional advice tailored to your needs. Staying informed and proactive empowers you to take control of your health and live a fulfilling life.