*This post may contain affiliate links for which I earn commissions.*
I understand you’re interested in how our emotional well-being impacts our physical health. It’s not just an intriguing topic; it’s fundamental to understanding our overall well-being. The notion that our minds and bodies are closely linked isn’t new, but it’s gaining broader acknowledgment in scientific circles.I’ll share with you what I have learned about the philosophy behind the powerful connection between our emotions and our physical state. We’ll explore how maintaining emotional balance is pivotal to our overall health. The idea to explore is that many physical illnesses may stem from emotional turbulence – essentially, that our feelings could significantly influence our susceptibility to disease.
What’s intriguing is the growing endorsement from the medical community. Researchers are increasingly investigating the ways chronic stress, unresolved trauma, repressed emotions, or detrimental thought patterns can actually translate into physical ailments – from something as benign as a cold to conditions as serious as heart disease.
By the end of this section, you’ll have a clearer understanding of the fundamental concepts that frame the intricate tapestry of the mind-body relationship. This sets the stage for the next part, where we’ll delve into the historical and current perspectives that bring to light the emotional origins of illnesses.
Why We Get Sick
What’s intriguing is the growing endorsement from the medical community. Researchers are increasingly investigating the ways chronic stress, unresolved trauma, repressed emotions, or detrimental thought patterns can actually translate into physical ailments – from something as benign as a cold to conditions as serious as heart disease. The fundamental concept behind this is the intricate relationship between the mind and body This sets the stage for the next part, where we’ll delve into the historical and current perspectives that bring to light the emotional origins of illnesses.
Unveiling the Emotional Roots of Illnesses
For centuries, healers and philosophers have pondered the connection between our emotional and physical states. Ancient medicine often addressed the whole person, considering emotional disposition as integral to diagnosis and treatment. Fast forward to today, and modern science is providing compelling evidence to support this age-old wisdom.
Fascinating research in psychoneuroimmunology, a field that studies how the brain and immune system interact, reveals how states like depression and anxiety can lower immunity, making us more susceptible to illness. Psychologists and medical doctors alike are uncovering patterns indicating that our emotional history may have a lasting imprint on our physical health.
One notable example comes from research demonstrating that patients with chronic illnesses, such as autoimmune diseases or cardiovascular conditions, often report long-term emotional distress predating their diagnoses. These cases serve as vital signposts in our understanding of the emotional origins of illnesses, suggesting a much closer relationship between our feelings and our bodies than previously acknowledged.
Michael Lincoln has stated that every organ has an emotion behind it. For instance, not dealing with unresolved grief will affect the lungs.
Grief/ – Lungs:
- Grief, especially when it is unprocessed or unresolved, affects the lungs. This can manifest in physical symptoms such as respiratory issues, asthma, or persistent colds. The lungs are seen as the organ responsible for taking in and letting go (breathing), and grief can hinder this process, resulting in stagnation and lung-related problems.
Anger – Liver:
- Anger and frustration are often associated with the liver. The liver is responsible for the smooth flow of energy and emotions in the body. When someone experiences chronic anger or suppresses their anger, it can lead to physical issues like liver disorders, headaches, or high blood pressure.
Fear – Kidneys:
- Fear, especially chronic or deep-seated fear, impacts the kidneys. In TCM, the kidneys are considered the source of vital energy (Qi) and are associated with the water element, symbolizing adaptability, resilience, and willpower. This association can manifest in physical symptoms such as kidney problems, lower back pain, or issues with bladder function.
Shock – Gallbladder:
- Shock, whether from sudden bad news, a traumatic event, or an unexpected life change, is believed to affect the gallbladder. In Traditional Chinese Medicine (TCM), the gallbladder plays a role in decision-making and courage. When a person experiences shock, it can disrupt the gallbladder’s function, leading to indecisiveness, hesitation, and difficulties in making clear choices.
Worry/Overthinking – Spleen:
- In Traditional Chinese Medicine (TCM), the spleen is associated with the emotion of worry and excessive mental activity. It is responsible for processing both food and thoughts, transforming nutrients into energy. When a person experiences excessive worry, overthinking, or rumination, it can disrupt the spleen’s ability to function optimally. This emotional strain weakens the spleen, leading to potential imbalances in the digestive system and energy distribution throughout the body.
Sadness/Depression – Heart:
- Explanation: In Traditional Chinese Medicine (TCM), the heart is more than just a physical organ responsible for pumping blood. It is also seen as the “seat of the mind” or “Shen,” representing the emotional and spiritual aspects of a person. The heart is associated with the element of fire, which symbolizes warmth, joy, and vitality. It is believed to govern our consciousness, thoughts, memory, and emotional well-being. Therefore, when we experience emotions of deep sadness or depression, it directly impacts the heart’s energy, leading to disruptions in both emotional and physical health.
Understanding How Stress Affects the Body
When I talk about stress, I’m not just referring to a bad day at work or a missed deadline. I’m discussing chronic stress, which is persistent and far-reaching, seeping into every aspect of life. A perpetual state of ‘fight or flight,’ chronic stress disturbs the body’s balance, wreaking havoc on nearly every system.
Here’s what happens: the body releases stress hormones like cortisol and adrenaline, which are meant for short-term survival scenarios. However, when these hormones flood the body on a prolonged basis, they can suppress the immune system, making you more susceptible to infections and diseases.
The impact does not stop there. Chronic stress is often linked with high blood pressure, heart disease, obesity, and diabetes. It can also intensify symptoms of other conditions. Learning to manage stress isn’t just good for your mind; it can literally help heal your body.
Practical stress management might include activities like yoga, deep breathing exercises, or therapeutic techniques designed to calm the mind and body. Regular physical activity, adequate sleep, and maintaining a healthy diet are foundational to reducing stress levels.
The way forward is clear – manage stress, and your body stands a better chance of staying healthy. But what about those deep-seared emotional wounds that are harder to spot and soothe? That’s where the role of trauma in physical diseases comes in, which we will explore in the next section.
The Role of Trauma in Physical Diseases
It’s become increasingly clear that trauma isn’t just a psychological scar; it can leave its mark on the body as well. Emotional wounds from traumatic events, particularly when unresolved, can lay the groundwork for a host of physical health issues. Trauma can stem from a variety of experiences, including abuse, accidents, loss, or any event that overwhelms an individual’s ability to cope.
When trauma affects our lives, it does so on multiple fronts. Our bodies respond to traumatic stress by entering a state of high alert, releasing a cascade of stress hormones like cortisol and adrenaline. This so-called ‘fight or flight’ response is crucial for immediate survival, but when it becomes chronic, it disrupts nearly every system in the body. It can inhibit immune function, heighten inflammation, and increase the risk of long-term health problems such as heart disease, diabetes, and autoimmune disorders.
Addressing trauma is key for healing, and this recognition has led to the development of various therapies. Conventional talk therapy, while useful, might not reach the deeper layers of trauma stored within the body. This is where body-centered approaches like somatic experiencing come in. By focusing on bodily sensations and movements, somatic therapy helps to release stored trauma, potentially easing the physical ailments linked to these emotional disturbances.
From Repression to Expression: Emotions and Illness
The link between unexpressed emotions and illness is not just a theory; it’s a reality many health professionals acknowledge. Unacknowledged grief, anger, or fear can take a significant toll on physical wellbeing. When emotions are buried, the body might ‘speak’ through illness, signaling the need for emotional release.
The risks that come with repressed emotions are substantial. They can contribute to various physical conditions, ranging from tension headaches to digestive issues. Moreover, psychological distress can exacerbate pre-existing physical ailments, complicating recovery and treatment.
Therapeutic methods like expressive therapies have shown promise in facilitating the release and processing of repressed feelings. Art therapy, music therapy, and writing can all serve as conduits for expression, often leading to powerful breakthroughs in both mental and physical health.
One example is the use of art therapy in cancer patients, which has been found to not only alleviate psychological distress but also to improve symptoms and quality of life. These testimonies support the view that releasing deep-seated emotions can have a transformative effect on health.
In transitioning from emotional inhibition to expression, it’s critical to approach this process gently. Rather than compelling the release of feelings, encouraging a natural flow of emotions can lead to a more profound healing journey.
As we explore these relationships, it becomes clear that embracing our emotional landscape is a pivotal step towards recovery and long-term health management. In the next segment, I’ll explore how mindfulness and somatic therapies further engage this process, emphasizing embodiment and awareness as keys to navigating the emotional origins of illness.
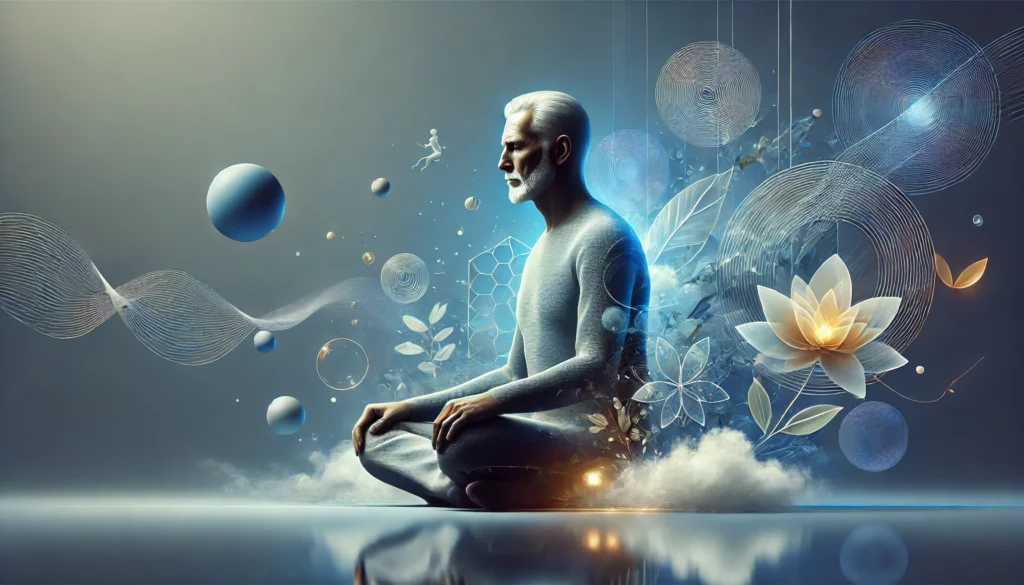
The core of mindfulness is cultivating an awareness of the present moment. By paying attention to thoughts, feelings, and bodily sensations without judgment, mindfulness practices can help individuals recognize and manage stress and emotional pain. Research substantiates its value, demonstrating that mindfulness can reduce symptoms associated with various conditions, such as chronic pain, depression, and heart disease.
Somatic therapy, on the other hand, integrates the mind, body, and spirit in a therapeutic context. It encompasses techniques that address physiological elements of trauma and stress by facilitating a connection between the body and emotional experiences. Through somatic practices, such as deep breathing, controlled movements, and body awareness exercises, individuals have found relief from tension and have been able to process emotions contributing to their illnesses.
Evidence supporting these therapies is growing. Clinical studies have shown reductions in the severity of symptoms, improvements in emotional regulation, and enhanced overall well-being among people engaging in these practices. This body of work is reinforcing the contention that emotional health is inseparable from physical health.
With the growing acceptance of these therapeutic approaches, healthcare professionals are increasingly incorporating them into treatment plans. This shift in perspective marks a critical step towards comprehensive healthcare, acknowledging the complex link between emotional and physical states.
Embracing mindfulness and somatic therapies can serve as a bridge to the next important aspect of healing: the transformation of negative thought patterns into positive ones. As we move into exploring how cognitive-behavioral therapy contributes to this process, we find that the power of the mind is not only a source of potential harm but also the strongest asset for recovery.
Challenging Negative Thought Patterns for Better Health
Negative thought patterns are like unwelcome weeds in the garden of the mind; they can overpower and crowd out healthier, more positive mental states. Recognition of these invasive thoughts is the first step in reclaiming mental and, consequently, physical health.
Cognitive-behavioral therapy, or CBT, is widely recognized for its effectiveness in identifying and altering destructive patterns of thinking. By applying CBT, individuals can systematically dismantle the thoughts that potentially weaken the immune system and exacerbate physical ailments.
The idea is to replace ‘cognitive distortions’ with more realistic and beneficial thoughts. Examples of distortions include: always anticipating the worst (catastrophizing), viewing situations in black-and-white terms (polarized thinking), and harshly labeling oneself over mistakes (mislabeling).
Through exercises, guided dialogue, and consistent practice, patients can rewrite the script of their internal narratives. This shift in mindset can lead to decreased stress and inflammation, both of which have direct correlations to physical conditions like heart disease and autoimmune disorders.
In fact, some remarkable recovery stories begin with patients tackling their psychological challenges. Improved mental wellness doesn’t just ease the mind’s burden but also allows the body’s natural healing processes to operate more effectively.
With better psychological resilience, we fortify our defenses against the common cold, reduce the risk of more serious illnesses, and generally promote a healthier existence.
Integrating Emotional and Physical Healthcare
It’s vital to consider emotional and physical health not as separate entities, but as intertwined components of overall well-being. Integrating emotional care with physical healthcare can create a more comprehensive treatment plan that addresses the multifaceted nature of illness.
Considering a person’s emotional state alongside their physical symptoms can lead to earlier identification of potential health issues. This holistic approach can prevent chronic conditions from worsening by tackling the emotional factors that may contribute to the disease’s progression.
Integrated care models foster collaboration between different healthcare professionals, including psychologists, psychiatrists, and general practitioners. This team-based approach ensures all aspects of a patient’s health are thoroughly evaluated and treated.
Success in integrated care is supported by patient education. Individuals are empowered to take an active role in their health when they understand the importance of emotional well-being in managing their physical conditions.
By considering case studies and qualitative data from patients who have benefited from integrated healthcare, we can draw valuable insights. These stories highlight the improved outcomes that are possible when emotional and physical health are treated concurrently.
Moving forward, the healthcare industry faces the challenge of standardizing integrated care, ensuring that it becomes more accessible and widely implemented. This shift will require not just changes in clinical practice, but also an evolution in healthcare policies and insurance coverage.
Future Horizons: The Evolution of Holistic Medicine
As I’ve explored the intricate web connecting our emotional states to physical health, it’s clear that the future holds immense promise for holistic medicine. The shift towards acknowledging the emotional origins of illnesses is not just a passing trend but a paradigm shift that has the potential to revolutionize how we approach healthcare.
Anticipating groundbreaking research in the field, medical professionals and scientists are increasingly advocating for more comprehensive studies that integrate emotional and psychological assessments into routine healthcare. This could transform diagnostic processes, ensuring that emotional well-being is evaluated alongside physical symptoms.
The development of new therapeutic techniques also seems imminent. Therapies that once stood on the fringe of medicine, such as mindfulness-based stress reduction and somatic experiencing, are now gaining ground as essential components of healing. As these practices become more mainstream, we might see a more harmonious blend of conventional and alternative medicine, providing a truly integrated approach to health.
In a world that’s rapidly recognizing the value of emotional health, it’s vital to stay informed and open to the ways holistic medicine can enrich our lives. Continued education for both healthcare professionals and patients is ESSENTIAL, fostering an environment where the mind-body connection isn’t just an idea, but a foundational aspect of wellness.
Imagine a healthcare system that not only treats the symptoms but also embraces the emotional narrative of each individual, offering treatments that address the whole person. It’s not just wishful thinking; it’s the direction we’re heading, and each step we take is a stride toward better health for all.